AQP4, AQP4 Antibody, and MOG Antibody
Reviewed by: HU Medical Review Board | Last reviewed: September 2021 | Last updated: September 2021
The symptoms that we now recognize as NMO were first described more than 100 years ago. However, without the right technology and testing, it was hard to separate NMO from other similar conditions, such as multiple sclerosis (MS).1
These diseases were originally thought to be one underlying condition with varying symptoms and severity. However, advancements in diagnosis and testing have allowed experts to find what makes NMO unique. One of these factors is the presence of specific antibodies. These are called AQP4 antibodies and MOG antibodies.1-4
What is AQP4?
AQP4 stands for aquaporin-4. It is a protein on the outside of certain brain cells. It controls water balance. Specifically, it controls how water moves in and out of cells. AQP4 can be found on cells in the brain, spinal cord, and along the nerve that controls vision (optic nerve).1,2,5,6
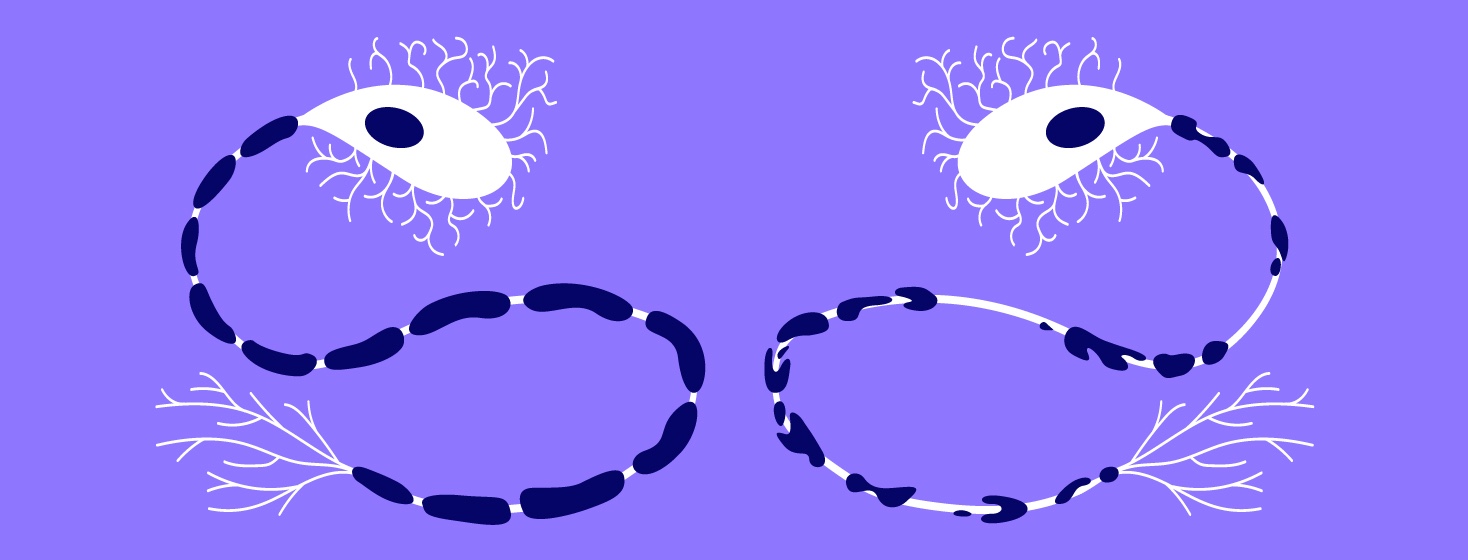
In the brain, AQP4 is found on cells called astrocytes. These play an important role in creating and maintaining the blood-brain barrier. This barrier protects the brain and spinal cord from many germs and toxins. Astrocytes also play a role in supporting nerve cells and communication between nerves. They help repair damage in the brain and provide nutrients. Astrocytes are the support cells of the central nervous system.5,6
The role of antibodies in NMO
NMO is considered an autoimmune condition. In autoimmune diseases, the body mistakenly attacks healthy cells, leading to symptoms. These attacks are carried out by antibodies. Antibodies are proteins our immune system makes. They have specific targets to protect us from germs. Antibodies can target different bacteria, viruses, and more. Our immune system depends on antibodies to keep us safe.1,2,5
However, sometimes these antibodies can make mistakes. Instead of targeting foreign invaders, they accidentally target normal cells. This can lead to damage and a variety of different issues depending on what normal tissue was attacked. Antibodies that attack healthy cells are called auto-antibodies.1
Although the exact way NMO develops is unknown, it is thought to be related to an issue with the blood-brain barrier, allowing auto-antibodies to enter the brain and spinal cord. These auto-antibodies can attack different cells, causing damage and inflammation. One area that is affected in NMO is the myelin sheath of nerves in the brain.1-6
The myelin sheaths protect nerve cells and allow them to communicate quickly with one another. Fast communication between nerves allows our body to carry out all the movements and functions it has to do. The process of destroying myelin is called demyelination.5
Demyelination leads to the symptoms of both MS and NMO. However, in NMO, new testing has shown that two specific autoantibodies are most often the cause of the changes and damage in this disease. In contrast, no specific antibodies have been discovered in MS. These two antibodies are AQP4 antibody and the MOG antibody.1-4
What is the AQP4 antibody?
The AQP4 antibody attacks the AQP4 protein. It is also called AQP4-IgG, or being AQP4-positive. About 80 percent of all people with NMO will have the AQP4 antibody. AQP4 antibody (AQP4-IgG) is not found in multiple sclerosis.1,3-6
The targeting of AQP4 to the brain, spinal cord, and optic nerve creates inflammation. This whole process leads to demyelination and the common symptoms of NMO like optic neuritis and transverse myelitis. Optic neuritis is inflammation of the optic nerve that causes eye pain and vision problems. Transverse myelitis is inflammation of the spinal cord that can lead to a variety of symptoms. Depending on which area of the spinal cord is affected, weakness, paralysis, problems with bladder function, sensory loss, and more can occur.1-5,6
What is the MOG antibody?
Along with AQP4-IgG, there is another antibody specific to NMO. This is called the myelin oligodendrocyte glycoprotein (MOG) antibody. It is also called MOG-IgG, or being MOG-positive. MOG is a protein on the myelin sheath. Antibodies against MOG lead to demyelination. MOG antibodies are less common in NMO than AQP4 antibodies.1,3,4
Although experts do not know all the differences between MOG- and AQP4-positive NMO, they have noticed some trends. For example, NMO caused by MOG antibodies affects men and women equally. This is different from AQP4-positive NMO, which affects more women. NMO with MOG antibodies is also more likely to involve both eyes at once and have fewer relapses. It is possible for a person with MOG-positive NMO to have only 1 episode. This is different from AQP4-positive NMO, in which a person is more likely to have multiple episodes of symptoms.1,3,4
For now, NMO is considered a spectrum of disorders that includes people with MOG or AQP4 antibodies, as well as those who are seronegative. However, some experts believe these should be separated into 2 different conditions. Further research into each type of NMO and the antibodies involved may provide answers to this debate in the future.
Do antibodies impact treatment?
Research into how NMO should be treated based on antibody type is ongoing. The AQP4 antibody is a relatively new discovery, and the MOG antibody is even newer. The most common treatment approaches for sudden attacks of both rely on high doses of corticosteroids (steroids). If this does not help, the next step is usually plasma exchange.1,5
For longer-term prevention of relapses, a variety of immune system-related treatments have been used. These include drugs that suppress the entire immune system or that target a specific step that blocks inflammation.1,5
However, in recent years, several drugs have been approved specifically for NMO with AQP4 antibodies. These include:1,7
- Enspryng™ (satralizumab)
- SolirisⓇ (eculizumab)
- Uplizna™ (inebilizumab)
As we learn more about AQP4, MOG, and other potential antibodies involved in NMO, drugs can become more targeted. Learning more about the different antibodies and how to test for them will also help lead to faster, more accurate diagnoses.
Were antibodies mentioned during the course of your diagnosis or treatment?
Join the conversation