The Challenges of Seronegative NMOSD
Neuromyelitis optica spectrum disorder (NMOSD) can have a variety of different symptom types, severities, and patterns. Since each person's experience with NMOSD is unique, it can be challenging to properly diagnosis the condition.
NMOSD was originally thought to be a type of multiple sclerosis (MS). However, new research and technologies have allowed for the development of new tools for diagnosis. Experts have discovered antibodies specific to NMOSD and have used these to separate it from MS.1-3
Finding these new antibodies and studying them in relation to a person’s symptoms has uncovered a wide spectrum of presentations that fall under the NMOSD umbrella. While a lot of progress has been made, there are still people whose symptoms do not fall neatly into some of these categories. An example of this is people who have seronegative NMOSD.
What are the main types of NMOSD?
As of 2021, the 2 main types of the condition are AQP4-IgG NMOSD and MOG-IgG NMOSD. AQP4 stands for aquaporin-4. This is a protein on the outside of certain brain cells that controls water balance. MOG stands for myelin oligodendrocyte glycoprotein. It is found on the myelin sheath of nerve cells. The myelin sheath allows nerves to communicate quickly with one another. IgG stands for a type of antibody.1-3
In AQP4-IgG and MOG-IgG NMOSD, the body makes antibodies that mistakenly attack healthy cells. Normally, antibodies are proteins that protect our immune system from germs. When they attack healthy cells, they can cause symptoms of NMOSD.1
It is more common to have AQP4-IgG NMOSD than MOG-IgG NMOSD. However, NMOSD is a spectrum of disorders and presentations. It is possible for 2 people to have AQP4-IgG NMOSD but have different severities of the condition.1-3
How is NMOSD diagnosed?
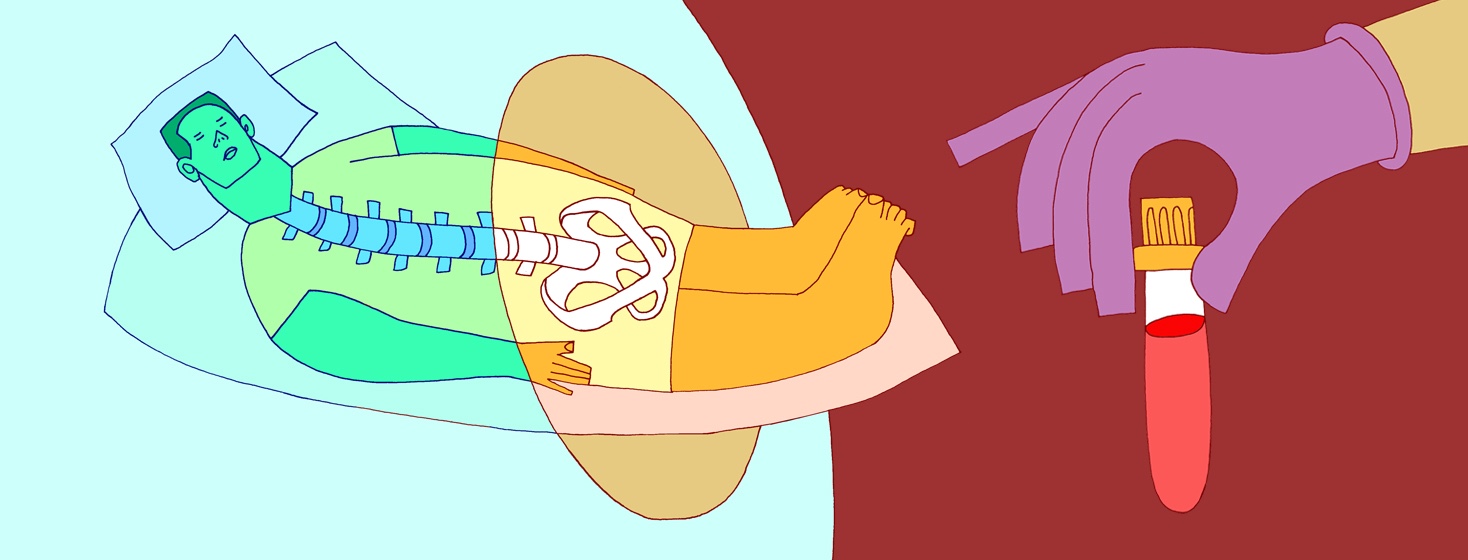
In order to diagnose NMOSD, your doctor will take a good symptom history. They will also perform a neurological exam. In most cases, they will do brain and spinal cord imaging with MRI (magnetic resonance imaging). This can help look for areas of damage.1,4,5
The unique part of diagnosing NMOSD comes from the antibodies. Your doctor can test for AQP4-IgG and MOG-IgG antibodies. Testing positive for one of these antibodies can lead to a faster diagnosis.1,4,5
For example, in order to diagnose AQP4-IgG NMOSD, a person needs to:1,4
- Test positive for AQP4-IgG antibodies on a blood test
- Have 1 or more of 6 key NMOSD features, such as optic neuritis (vision problems or eye pain) or area postrema syndrome (persistent hiccups, nausea, and vomiting)
- Have no other reasonable diagnoses
Therefore, with one or more key symptoms and a positive blood AQP4-IgG antibody test, the diagnosis can be straightforward.
What is seronegative NMOSD?
There is also a third type of NMOSD. This is called seronegative NMOSD. People with this third type do not test positive for the known NMOSD antibodies.1,7
There are several reasons why this might occur. First, it is possible that the test is a false negative. This means a person tests negative for an antibody but they actually have it. Some experts think false negatives could occur in as many as 1 in 5 people or more.6
Second, it is also possible that there are other antibodies that lead to NMOSD that we have not discovered yet. Before experts discovered MOG-IgG antibodies, people who would have tested positive for this antibody would have been considered seronegative.1-3,7
Finally, it is also possible that there are other causes of NMOSD besides specific antibodies. This would explain why a person would not test positive but still have classic symptoms.1-3,7
Challenges of seronegative NMOSD
Diagnosing seronegative NMOSD is not always straightforward. While there can be delays in diagnosing any case of NMOSD, seronegative may be the trickiest to pin down. There are additional requirements to be formally diagnosed with NMOSD if a person does not test positive for a specific antibody. These include:1,4
- At least 2 key NMOSD features, with at least 1 being optic neuritis or acute myelitis (inflammation of the spinal cord)
- Distinct differences in the key features that indicate damage across different areas of the nervous system (dissemination in space)
- Variety of different MRI findings in different areas of the brain depending on the specific symptoms present
- Exclusion of other diagnoses
Pinpointing several different key symptoms as well as observing specific, accompanying imaging findings can be tough. Fulfilling all of these requirements can make it challenging to diagnose seronegative NMOSD quickly and efficiently. It can also mean that a person experiences other misdiagnoses along the way.
Plus, because NMOSD is a spectrum of disorders with more information uncovered regularly, not all doctors agree on how to classify it. This can make the diagnostic process different based on what doctor you see.
Overall, seronegative NMOSD presents its own unique challenges. However, lots of progress has been made in recent years, and ongoing research is helping us to learn more.
Join the conversation